Why perform it?
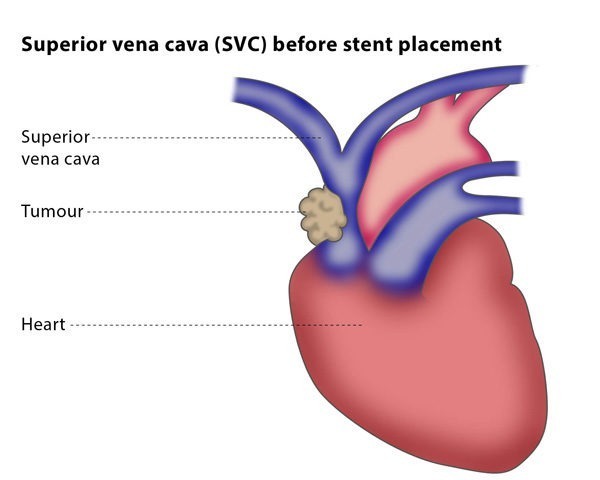
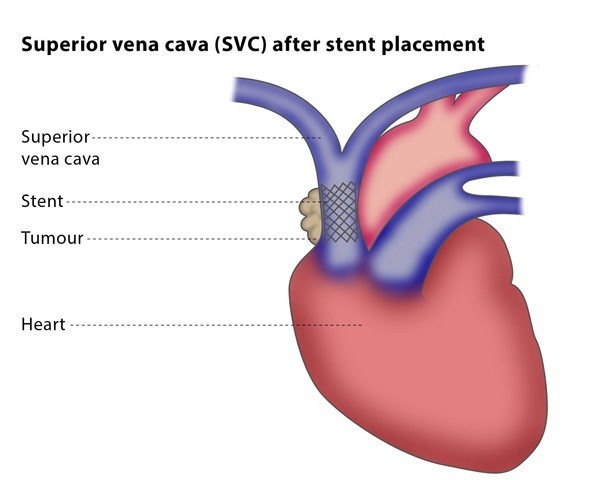
The aim of vena cava stenting is to manage symptoms caused by an obstruction of the blood flow in the vein, which is much more common in the SVC than in the IVC.
The main symptom of an obstructed blood flow in the vena cava is shortness of breath, followed by swelling of the face, neck or arms, a headache, a cough and enlargement of the veins in the neck, chest and arms. You may experience other symptoms but they are rare.
Your symptoms should stop within 48 hours of the stent placement.
What are the risks?
There are some minor risks, including the risk of infection and bruising at the puncture site in your neck or groin. Major risks include the risk of the stent accidentally going into the heart during placement, the development of a blood clot, or the stent later becoming blocked due to a tumour, though in this case the vessel can be reopened in a second intervention.
Bibliography
1. Nagata T, Makutani S, Uchida H, Kichikawa K, Maeda M, Yoshioka T, Anai H, Sakaguchi H, Yoshimura H. Follow-up results of 71 patients undergoing metallic stent placement for the treatment of a malignant obstruction of the superior vena cava. Cardiovasc Interv Radiol 2007; 30:959-967.
2. Rizvi AZ, Kalra M, Bjarnason H, Bower TC, Schleck C, Gloviczki P. Benign superior vena cava syndrome: stenting is now the first line of treatment. J Vasc Surg 2008; 47:372-380.
3. Ploegmakers MJ, Rutten MJ. Fatal pericardial tamponade after superior vena cava stenting. Cardiovasc Intervent Radiol. 2009 May; 32(3):585-9.
4. Albers EL, Pugh ME, Hill KD, Wang L, Loyd JE, Doyle TP. Percutaneous vascular stent implantation as treatment for central vascular obstruction due to fibrosing mediastinitis. Circulation. 2011 Apr 5; 123(13):1391-9.