Clinical Services in IR Task Force
Clinical services in IR
While the set-up of interventional radiology as well as IR’s access to the three pillars of clinical practice – infrastructure, staff and time – varies considerably across Europe, CIRSE encourages all interventional radiologists to put more consideration towards their clinical practice. Every IR can begin to develop their own clinical practice by starting to do patient rounds before and after a procedure. In most cases, it has been or will be an incremental and often long process from patient rounds towards outpatient clinics and potentially inpatient IR beds, but it will be worth the journey.
Following the publication of the CIRSE Clinical Practice Manual in 2021, a dedicated task force was established in 2023 to advance IR as a clinical specialty. This task force will assess the status quo of clinical practice in IR, develop strategies for setting up a clinical service in IR considering varying framework conditions, and contribute to broadening CIRSE’s educational offer in this field.
Click here to view the members of the Clinical Services in IR task force.
The future is clinical, and the best time to start your IR clinical service is now!
Watch Prof. Binkert’s CIRSE 2023 speech on CIRSE’s vision for the future of interventional radiology here.
Toolkit for IRs
The Clinical Services in IR Task Force has compiled a toolkit for IRs at all stages of their career – offering practical advice, training, and education materials as well as further readings for specific topics. IRs are invited to use these tools to improve their skills or master challenges or opportunities they are currently facing.
CIRSE Academy course
The CIRSE Academy course on clinical practice, authored by J. Chun and S. Duvnjak, corresponds to chapters 2.1.5, “The interventional radiology team” and 2.1.6, “Interventional radiology clinical practice” in the European Curriculum and Syllabus for Interventional Radiology.
Learning objectives:
- To understand the necessity of developing and maintaining an IR clinic to evaluate patients pre- and post-procedure; provide information and obtain informed consent in advance of procedures; effectively communicate and build a rapport with patients and to properly assess outcome measures.
- To promote effective teamwork within the hospital to facilitate obtaining relevant clinical advice for patient management and to understand the importance of attending relevant multidisciplinary team (MDT) meeting.
- To understand the mechanisms for continually monitoring quality assurance including regular documentation and classification of complications from IR procedures and regular morbidity and mortality meetings.
CIRSE Library topic packages
- Clinical practice building in IR – compiled by A. Mahnken and S. Duvnjak in April 2025
- Provision of IR Services – compiled by C. Nice in April 2023
Micro-education videos
The following videos are designed to provide very practical information on basic topics regarding clinical practice in IR in a concise manner. More videos will be available soon.
How to speak to your patients
The Clinical Services in IR Task Force has launched the pilot of its new micro-education series, which will help you get your clinical practice up to speed. Theses short and very practical videos will allow you to easily master the essentials of clinical engagement!
For our first video, we talked to CIRSE Clinical Practice Task Force member Prof. Thierry de Baere for some tips and tricks on how to get more clinically involved in interventional oncology by improving communication with your patients.
How to make the most MDT meetings
Watch this video for valuable tips and tricks from Dr. Joo-Young Chun from St. George’s Hospital in London on how to best contribute your knowledge to multidisciplinary team meetings for the best patient outcome.
How to obtain informed consent
In this video, Clinical Services Task Force member Prof. Miltos Krokidis explains how to inform your patient about an indicated procedure and how to take informed consent.
How to assess a patient
In the third video of this series, Clinical Services in IR Task Force Chairperson Prof. Andreas Mahnken explains the basics you need to know about how to assess a patient, with the example of portal hypertension.
How I started my outpatient clinic
In this video, Dr. Daniel Kütting offers advice on how to successfully set up an outpatient IR clinic.
How to take a patient history in IR
In this part of our series, Prof. José Urbano gives tips and tricks on how to take a patient history in IR.
How to speak with paediatric patients
In this video, paediatric specialist Dr. Alex Barnacle gives tips and tricks on how to with a few simple changes, you can adapt your clinical practice to better fit the needs of paediatric patients.
Documentation
Watch this video for valuable tips and tricks from task force member Dr. Joo-Young Chun on how to improve the documentation workflow in your department.
CIRSE webinar
Watch this deep dive into clinical practice with some of CIRSE’s greatest experts on the topic.
CIRSE Webinars: Get your clinical practice up to speed
This webinar features an introduction to the CIRSE Clinical Practice Manual, an analysis of the clinical practice survey results, and an exploration of CIRSE’s comprehensive understanding of clinical practice activities. It also includes in-depth discussions on conducting patient assessments and examinations, with a focus on the specific considerations for vascular versus interventional oncology patients.
This webinar and all CIRSE webinars are available to watch via the CIRSE Library!
CIRSE Webinars: Get your clinical practice up to speed
This webinar features an introduction to the CIRSE Clinical Practice Manual, an analysis of the clinical practice survey results, and an exploration of CIRSE’s comprehensive understanding of clinical practice activities. It also includes in-depth discussions on conducting patient assessments and examinations, with a focus on the specific considerations for vascular versus interventional oncology patients.
This webinar and all CIRSE webinars are available to watch via the CIRSE Library!
Additional resources
The Task Force has furthermore compiled relevant further readings a list of arguments in favour of building clinical practice in IR, supported by relevant references, that IRs can consult for negotiations with their hospital administration or regulatory bodies.
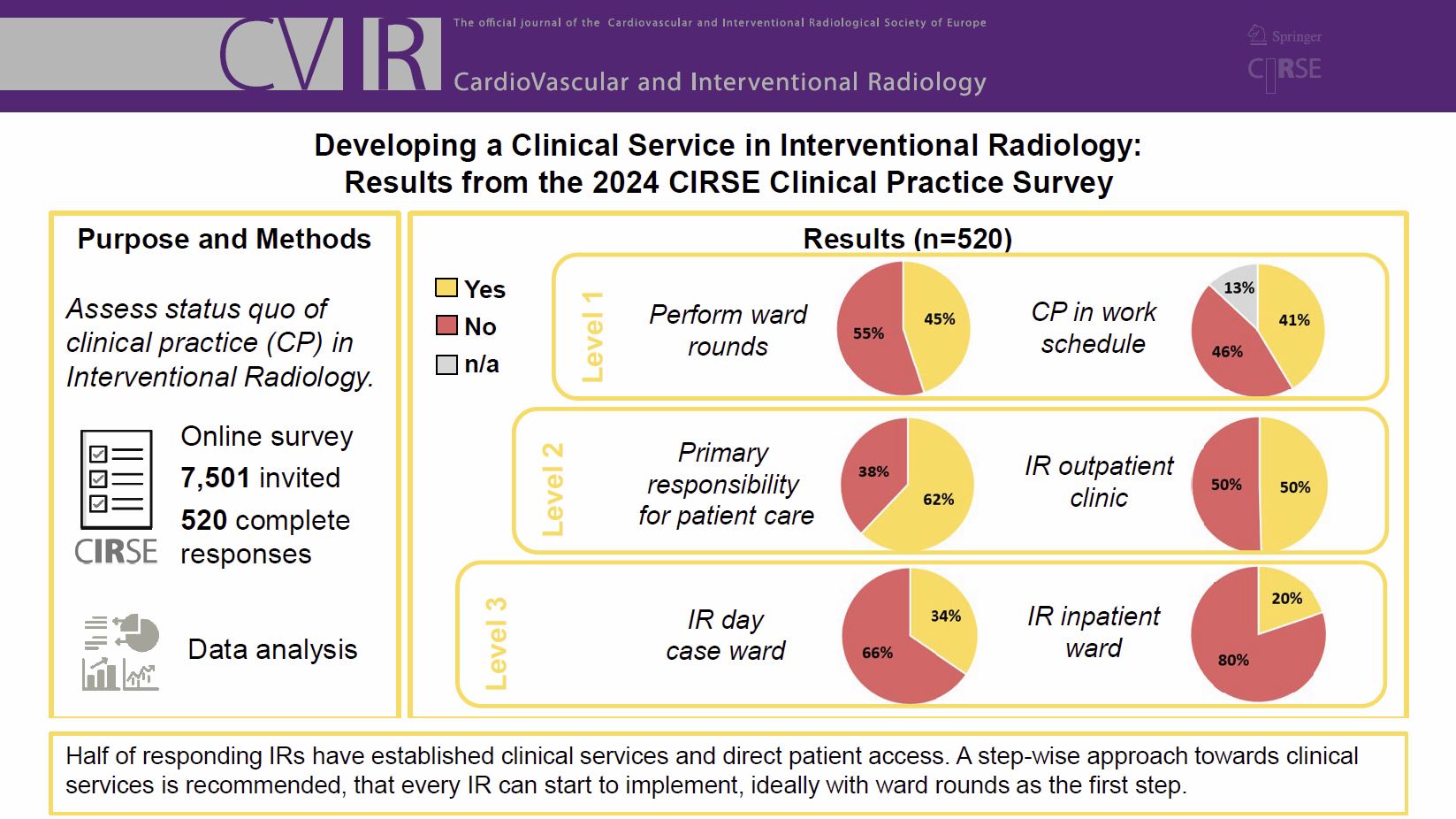
Read up on the current status of clinical practice in interventional radiology in the recently published article “Developing a Clinical Service in Interventional Radiology: Results from the 2024 CIRSE Clinical Practice Survey.” Download it here.
Levels of clinical services infrastructure
The Clinical Services in IR Task Force developed a three-stage system for clinical services infrastructure development. This system shall help create awareness of the fact that different levels of service provision can be offered and worked towards. IRs may also use this system to benchmark themselves and set personal goals for future developments in their centre and practice.
Inpatient
- Regular visits to all patients treated by IR (IR rounds – making/suggesting prescriptions)
- Preprocedural (work up and/or) communication with patients
- IR takes part in relevant MDT (vascular/oncology) meetings
Outpatient
- IR sees and treats outpatients without own outpatient clinic/infrastructure
- Preprocedural work up and/or communication with patients
- IR takes part in relevant MDT meetings (vascular/oncology) meetings (if applicable)
All of the above, plus
Inpatient
- Dedicated Time for clinical work in IR
- Ordering/performing clinical work e.g. blood sampling, clinical exam etc. beyond IR procedures
- Admission rights (without own beds)
- Standard operating procedures (SOPs) for most common procedures
Outpatient
- Dedicated Time for clinical work in IR
- Ordering/performing clinical work e.g. blood sampling, clinical exam etc. beyond IR procedures
- Limited IR outpatient clinic
- Standard operating procedures (SOPs) for most common procedures
- IR referral pathways/ entry point (e.g., admission desk)
All of the above, plus
Inpatient
- Regular ward rounds
- Own beds (revenue is assigned to IR)
- Dedicated IR theatre staff / physician support staff
- Independent access to hospital resources (e.g., imaging, laboratory, pathology, etc.)
- Training scheme/programme for IRs and staff
- Regular M&M meetings as part of governance
Outpatient
- IR Outpatient clinic with dedicated IR staff (revenue is assigned to IR)
- Independent access to hospital resources (like imaging lab etc.)
- Training scheme/programme for IRs and staff
- Regular M&M meetings as part of governance
- IR day unit – independent day case pathway from referral to follow-up
For any further information about CIRSE’s activities in the field of clinical practice as well as the task force’s work, please contact [email protected].
Task force members
| Name | Role | ||
|---|---|---|---|
| Andreas H. Mahnken | Chairperson | ||
| Alessandro Cannavale | |||
| Joo-Young Chun | |||
| Thierry De Baere | |||
| Rok Dezman | |||
| Stevo Duvnjak | |||
| Miltiadis Krokidis | |||
| Maria Antonella Ruffino | |||
| Anthony Ryan | |||
| Jose Urbano | |||