CIRSE Fellowship report: Dr. Ali Cantürk
My name is Ali Cantürk, MD, and I am a consultant radiologist at the Department of Radiology, Abdülhamid Han Training and Research Hospital in Istanbul, Turkey. I completed my residency in diagnostic and interventional radiology at Dokuz Eylül University in 2024 with a strong motivation to pursue a career in interventional radiology. In August 2025, I had the privilege of participating in the CIRSE Fellowship Programme, spending one month at the Royal Marsden Hospital in London under the mentorship of Prof. Nicos Fotiadis.
Fellowship experience
During my fellowship, I had the opportunity to work closely with Prof. Fotiadis, as well as with Dr. Nasir Khan and Dr. Edward Johnston. I also benefited greatly from the support of senior fellow Dr. Emma Dunne and colleagues Dr. Karthik Rajendran and Dr. Peter McAnena. Their expertise, guidance, and collegial spirit made my integration into the department both smooth and productive.
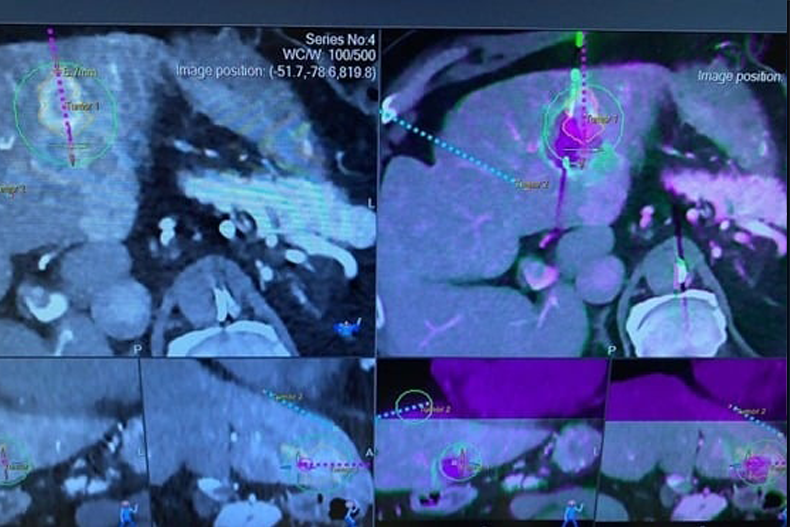
The Royal Marsden is a world-renowned oncology hospital, and its exclusive focus on oncological patients exposed me to a wide spectrum of interventional oncology procedures. These included robotic ablations of the liver, lung, and kidney; robotic biopsies; biliary interventions; transarterial embolizations; urinary interventions; and various ablative therapies. In particular, I broadened my knowledge of ablation modalities such as microwave ablation, radiofrequency ablation, and cryoablation, gaining valuable insight into how each technique is selected and applied according to patient- and tumor-specific factors. One especially innovative technique was transcatheter CT hepatic angiography for liver ablation, which allows highly precise delineation of ablation margins and demonstrates how advanced imaging enhances both precision and safety in interventional oncology.
Beyond routine procedures, I was able to observe complex ablations in detail. These highlighted how factors such as tumor size, location, and proximity to vital structures influence both the choice of ablation modality and the overall therapeutic approach. Watching the planning and execution of these cases gave me a deeper understanding of how interventional radiology can be tailored to maximize efficacy while ensuring patient safety.
Multidisciplinary and organizational insights
Another valuable aspect of my fellowship was experiencing the workflow and organizational structure of the interventional radiology unit. Every morning at 8:50 am, the team gathered for a planning meeting where patient cases, anesthesia, positioning, and potential challenges were reviewed in detail. These sessions were not routine briefings but genuine multidisciplinary exchanges in which every team member contributed. For me, this highlighted how a well-structured start to the day optimizes workflow, enhances safety, and strengthens teamwork.
I also attended multidisciplinary tumor board meetings, where oncologists, surgeons, pathologists, and interventional radiologists discussed complex cases together. These boards ensured that every perspective was considered, and treatment strategies were shaped by consensus. I was impressed by the respect and collaboration across specialties, which ensured patients received individualized treatment plans. These meetings reinforced that interventional radiology must operate as an integrated part of cancer care rather than in isolation.
Another key observation was the department’s patient-centered approach. Informed consent was clear and comprehensive, patients were treated respectfully, and structured follow-up protocols were in place. Standardized checklists and clearly defined responsibilities ensured continuity of care from admission to discharge. These experiences underlined that, alongside technical expertise, communication and organization play a vital role in delivering safe and effective care.
The hospital’s infrastructure also supported high-quality practice. Advanced angiography suites, hybrid imaging facilities, and dedicated recovery areas reflected a system designed around safety and efficiency. Seamless collaboration between radiologists, anesthesiologists, nurses, and radiographers created an environment that made it easier for me to adapt and feel fully integrated into the team.
Personal experience
Living in London for a month was an unforgettable experience. The city’s cultural richness, vibrant parks, and historical landmarks provided opportunities to reflect and recharge outside of the hospital. I left with a strong desire to return, both to the hospital and to the city.
This fellowship not only strengthened my technical knowledge but also broadened my perspective on patient care and workflow organization. Observing the high standards at the Royal Marsden inspired me to bring similar approaches back to my home institution, particularly regarding structured daily planning, multidisciplinary collaboration, and patient-centered communication. I also gained a deeper understanding of ablative techniques—especially microwave ablation and cryoablation—and how these can be tailored to individual patients. The insights I gained into patient selection and complication management will significantly influence my practice going forward.
Acknowledgements and conclusion
I am especially grateful to my mentor, Prof. Nicos Fotiadis, for his close guidance and invaluable teaching, as well as to Dr. Nasir Khan, Dr. Edward Johnston, and Dr. Emma Dunne for generously sharing their expertise. My sincere thanks also go to Dr. Karthik Rajendran and Dr. Peter McAnena for their support, which made my stay both productive and enjoyable.
I would also like to thank Shaira Farooq, who supported me from the very first day and ensured I felt comfortable and integrated. Finally, I extend my gratitude to the entire Royal Marsden IR team, including the nurses and radiographers, for their professionalism, kindness, and constant willingness to help.
This one-month fellowship at the Royal Marsden Hospital has been a transformative experience that will significantly shape my professional practice in interventional oncology. It enriched not only my technical and clinical expertise but also my appreciation for teamwork, workflow organization, and patient-centered care. I am eager to share the insights I gained with colleagues in Turkey and to contribute to the advancement of interventional oncology in my country.
I am profoundly grateful to CIRSE for making this opportunity possible. By supporting young interventional radiologists with access to leading European centres, the fellowship programme plays a vital role in fostering education and international collaboration in our field.