What is an infiltration and guided injection?
In between the vertebrae in your spine there are spinal discs (also known as intervertebral discs), and in the middle of each spinal disc is a jelly-like substance which is called the nucleus pulposus. Occasionally, the nucleus pulposus bulges through the outer ring which normally keeps it in place. This is known as herniation of the intervertebral disc or a ‘slipped disc’ and is a major cause of lower back pain, affecting mobility, physical function and quality of life.
Facet joint syndrome is another form of chronic lower back pain. It is characterised by stiffness and pain that increases when twisting and bending backwards. It is frequently caused by osteoarthritis, a type of arthritis that causes joint cartilage to deteriorate. This can also be caused by the joints bearing an unusual amount of weight as well as by repetitive stress injury. Facet joint syndrome is not easy to diagnose because it may be unclear where the source of the pain is located, making it easy for symptoms to be confused with the many other causes of back pain.
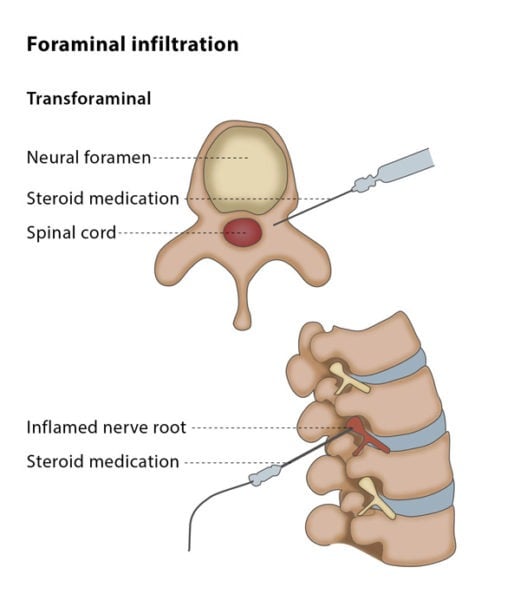
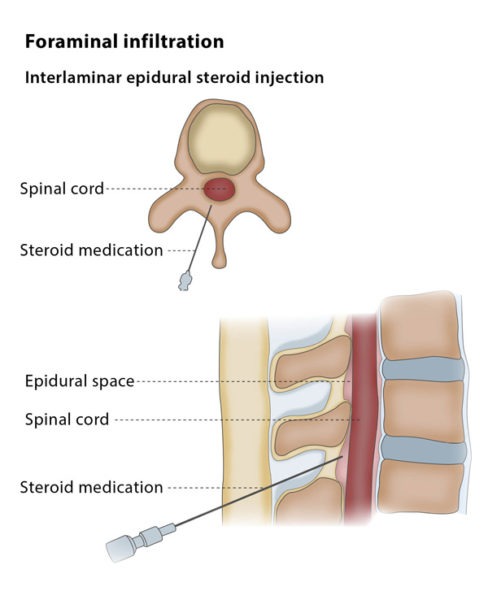
An infiltration and guided injection is the injection of local anaesthetics, steroids or ozone into your lower back for the treatment of sciatic pain due to disc herniation or facet joint syndrome. The procedure can be done under fluoroscopy or CT guidance.