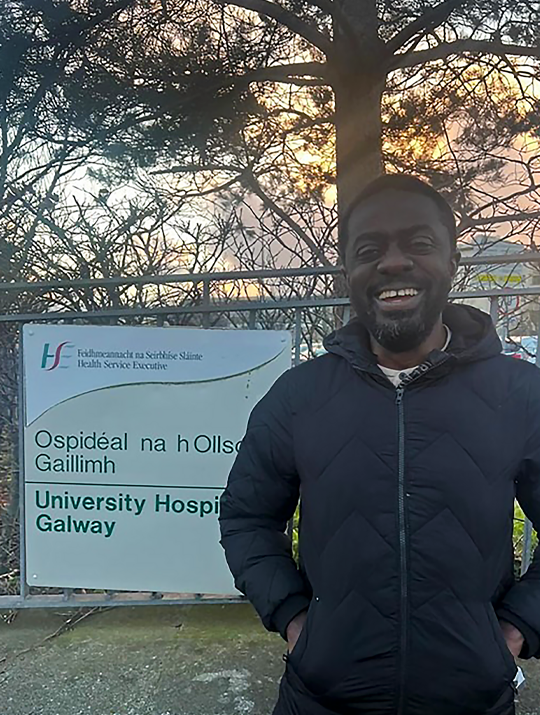
CIRSE Fellowship report: Agboola Said Ajibola
My name is Agboola Said Ajibola, and am an interventional radiologist from Nigeria. I completed my CIRSE fellowship grant program at Galway University Hospital (GUH), Ireland, under the supervision of Dr. Cormac O’Brien.
I applied to GUH because of the outstanding venous and arterial embolization work being carried out there, as these are areas in which I hope to gain proficiency. As an Interventional Radiologist, I am particularly interested in venous procedures, uterine artery embolization, and dialysis fistula work. I was especially excited to meet and work with Prof. Gerard O’Sullivan, who is world-renowned for his venous work in interventional radiology.

With Dr. Cormac O’Brien (in the blue sweater) and the rest of the IR team at GUH
Upon my arrival at the University of Galway Interventional Radiology Department, I met Dr. O’Brien, who was very welcoming. He introduced me to the team and, almost immediately, I was given scrubs, and we began work.
My first day was a whirlwind, as we had seven cases: two gastric tube placements, one biloma drainage, two liver biopsies, one psoas abscess drainage, a PICC line placement, and an inferior epigastric artery embolization. This was an excellent experience for me, as I was able to observe procedures that are not routine in my home center or during my fellowship training.
I had firsthand exposure to DVT thrombectomy cases with Prof. O’Sullivan, using relatively novel devices in patients with in-stent stenosis. We performed mechanical thrombectomy and angioplasty with satisfactory post-procedure venography results. I also assisted in the deployment of an IVC filter in one of the procedures.
There were several other amazing attendings I worked with, including Drs. Shepard, Davidson, and Mullins, all of whom were accommodating and eager to teach. We performed procedures such as varicocele embolization, chemoport placement, and fistula declotting.
I assisted Dr. O’Brien with my first ureteral stent placement, a procedure usually performed by urologists at my center. I also observed PICC line placement using ultrasound and an ECG-guided device instead of fluoroscopy.
I must add that the rest of the team — nurses Marie, Eliane, Vimbai, and Steve, as well as techs like Ola and others — made my stay pleasant and productive. They helped me understand dressing kits and the advanced functions of the fluoroscopy machine.
Dr. Cormac O’Brien ensured I had a well-rounded experience by involving me in weekly multidisciplinary meetings with the vascular surgery department, where complex aortic cases were discussed. I also visited the vascular lab, where patients were evaluated using Doppler ultrasound and ABI. This was my first exposure to the ABI machine.
One of the major reasons I chose Galway was its expertise in venous procedures, and I am pleased to say that this goal was achieved based on the cases I observed and the access I was granted to previous venous procedures.
I recently performed a catheter-directed thrombolysis (CDT) on a 31-year-old patient with cavo-ilio-femoral DVT. Before initiating the CDT, I deployed an IVC filter, which was from the same manufacturer as the one I used in Galway. I was able to perform this procedure confidently due to my exposure to similar cases at GUH. As a result, this and similar cases are now established procedures in my practice.
Whereas interventional radiology (IR) at GUH is well established, with multiple interventionists, IR nurses, and technologists, I am currently the only interventionist at my center and am in the process of building an IR team. Consequently, I observed closely how the process at GUH is carried out—from when a patient’s request is submitted for IR review, to imaging review, case booking, patient preparation by the nurses, and post-procedure site dressing. I have adopted this system to ensure a better workflow at my center.
I am particularly pleased with the dressing kits used at GUH, and one of the first steps I took was to advise my management and nursing staff to obtain similar kits, as they are more patient-friendly in terms of comfort and reduced risk of dislodgement, a common complication in IR procedures involving tube placement.
Medical Innovation floor at Galway Museum

Lovely sight along the streets of Galway
A major difference between my practice and that of GUH is that I have a dedicated clinic day to see patients, whereas at GUH, colleagues often come in to discuss cases directly with the interventionist. I now also welcome colleagues to discuss patient cases with me directly, rather than strictly requiring referrals to my clinic, as I believe both approaches have their own merits and limitations.
Outside of IR and GUH, I was able to explore Galway. I tasted Irish fish and chips, visited the Galway Museum, learned about the city’s history and the Spanish Arch, and saw impressive medical device innovations displayed there.
My experience in Galway can best be described as the most enriching four weeks of my budding interventional radiology career. I return to Abuja, Nigeria with valuable experience, improved skills, and greater confidence. The highlight was receiving an open invitation from Prof. O’Sullivan to return for further training, as well as opportunities for future collaboration with Drs. O’Brien and Mullins.
Thank you, CIRSE, for such a wonderful opportunity.