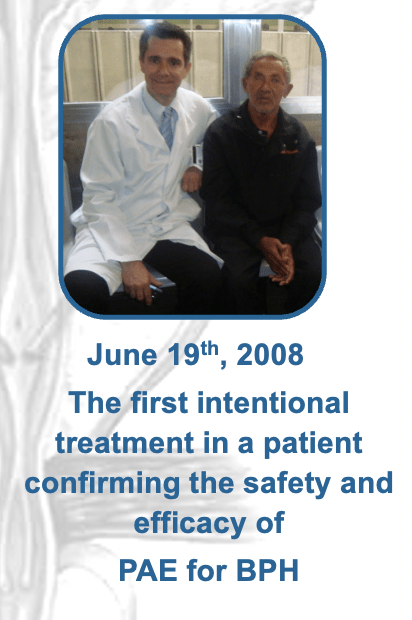
Both patients were too high-risk to operate on due to comorbidities, and had had Foley catheters in place for nearly a year. After writing the protocols and assembling a team which included radiologists, pathologists, urologists, radiologists and IRs, we offered prostatic artery embolization to the patients. They accepted the idea, we treated them, and they were able to remove the Foley catheters after treatment. Now, we had proved that PAE was safe and effective to treat patients suffering from complications related to the BPH-enlargement.
We submitted our results to CVIR, and it was a huge honour for myself and my team at the University of Sao Paolo that they were accepted and published in 2010. I presented on PAE at CIRSE for the first time that year, in Valencia 2010. One year later, we published the mid-term results in CVIR, and we started to develop a programme for treating patients with PAE. With teamwork, and under the supervision of the urology department, we started to get really good results. Even with the urology chairman’s support, you can imagine there was a huge resistance from the urology community, and I made a few enemies.
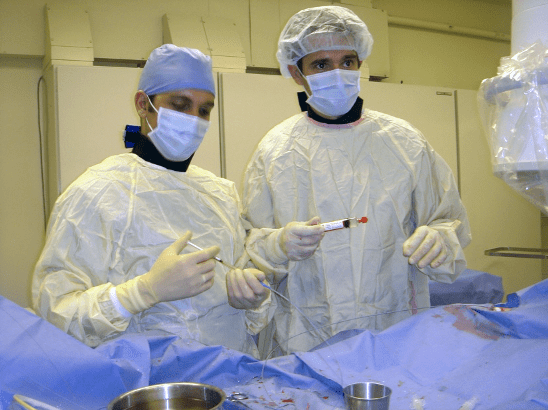
I started to travel around giving talks on PAE, and also training physicians in this technique. I had physicians from the world over come to me in Brazil, and travelled to other hospitals in the endeavour to replicate this procedure across the globe. It was surreal, to begin teaching internationally known IRs. I was used to going to medical meetings, to CIRSE and SIR, watching these great physicians presenting and teaching everyone. Then one day, I was teaching them in my life, in my patients, and they were there doing the procedures with me. It was an honour and a pleasure to host them at the University of Sao Paolo. It was also wonderful because they were able to give their valuable inputs on the procedure to me.
Thanks to the attention that sprang from teaching so many great physicians, I got the invitation to do a live case. It was one of the greatest things that happened in my life – and then it was really terrible. Soon you’ll understand why!
I was invited to transmit a live case from the Syrian Lebanese Hospital in Sao Paolo to New York City for that year’s GEST meeting, organized by Jafar Golzarian and Mark Sapoval. It would be the very first PAE procedure transmitted live. I was in New York alongside my urologist, and my team, coordinated by Airton Mota, MD, did the procedure at home in Sao Paolo.
My team talked to the most important TV channel in Brazil and asked if they would like to cover the case. A Brazilian surgery was going to be transmitted, live, to New York, USA! They were interested, and so the TV channel went to the hospital, and during the live transmission to New York, they were also transmitting the story to Brazilian TV and – wow. It was great!
After the live case and the subsequent discussion, my cell phone rang. It was the CEO of Syrian Lebanese, and he told me “Hey, Francisco, we have 1000s of calls to our hospital. The entire population was watching TV, and they want to be treated by this procedure.” BPH is a very common disease. Around 50% of men will have BPH symptoms of urinary obstruction after their 60s. The telephone lines of the hospital were completely blocked, but that night I told the CEO, let’s try to set these patients in the ambulatory clinic of the hospital. It’s important. We’ll see these patients with urologists.
Later, while still in New York, I got an email. “Dr. Carnevale, as soon as you get back to Brazil, we urgently need a meeting with the board of the hospital and with urologists of the hospital. There was a movement from some urologists in the hospital telling us that you have done a procedure that was not allowed in the country. It seems you have done something illegal.”
In a short span of time, I went from the top of the world to the precipice of being fired from not only Syrian Lebanese, but also from the University of Sao Paolo – as I mentioned, they are very close and work together. I was about to be fired with the idea that I was doing something illegal. But it was not illegal!
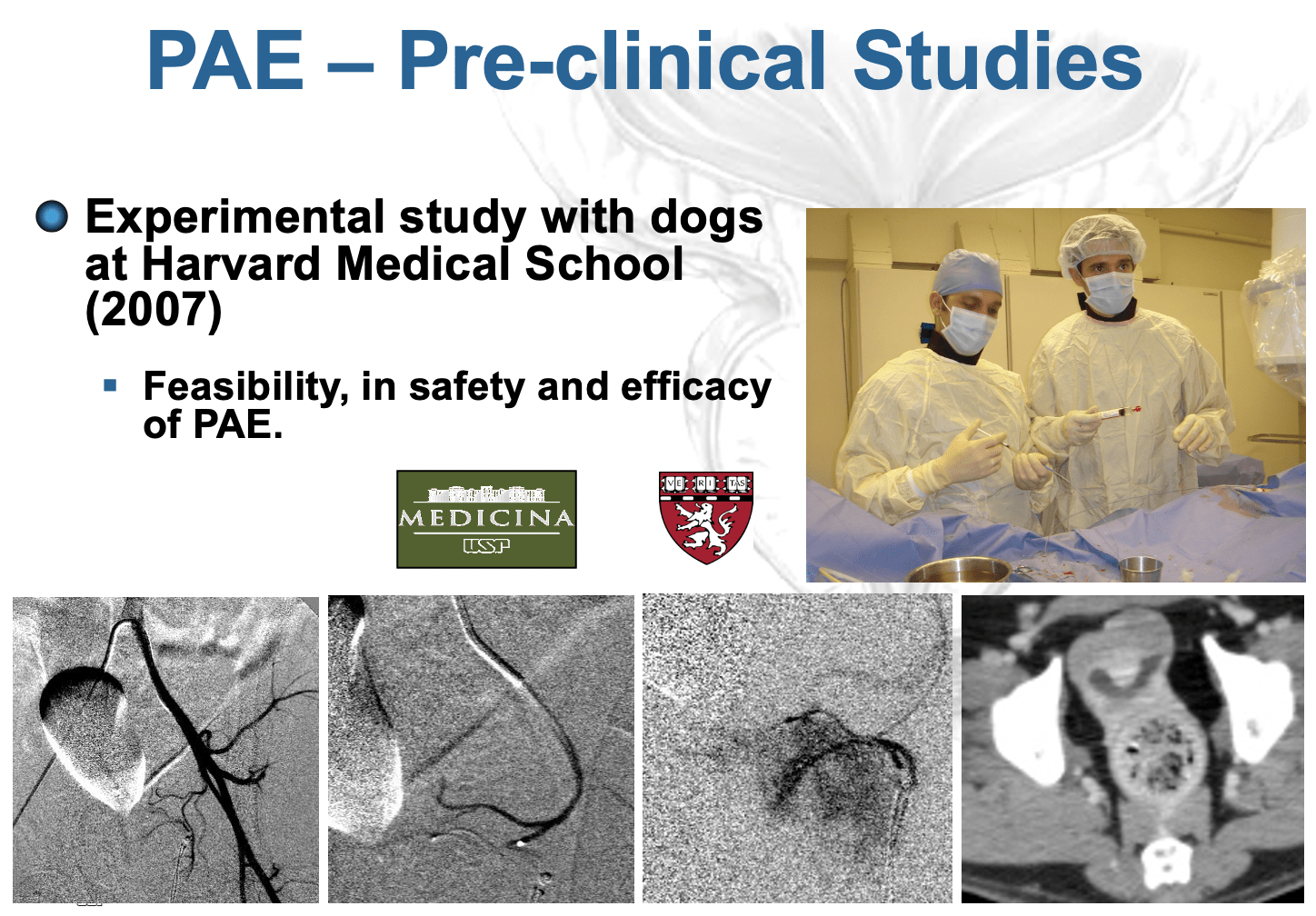
We had the code of embolizing a tumour, embolizing haematuria. The hospital was aware of everything. So, I wrote a dossier several hundred pages long and submitted it to the Federal Council of Medicine in Brazil (Pictures 6 and 7), which is the highest level I could escalate to. The dossier had everything, every bit information from the very first experimental and clinical studies up until the present to prove that I had done nothing illegal.