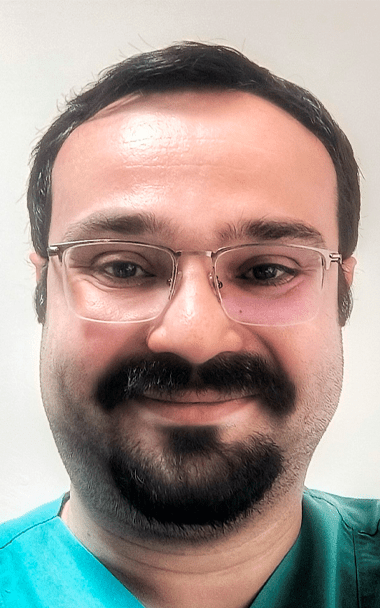
Dr. Bibin Sebastian from St. Gregorios Advanced Interventional Radiology Services
Parthanamthitta, India
“I was lucky enough to be inspired by my mentors to recognise the potential of IR to develop as a standalone speciality. After my basic IR fellowship in India, I pursued extensive training in the UK, which helped me gain the confidence and expertise to set up a dedicated IR department. This allowed us to offer innovative, minimally invasive IR treatments to our patients under one umbrella.
Now, as we are nearing 100 days of St. Gregorios Advanced Interventional Radiology Services (STAIRS), we offer novel IR treatments to patients including out-patient consultations, workups, diagnosis, and management. We work as any other independent speciality in this hospital.
Initially, convincing the hospitals about the need for an independent IR department was a challenge. However, I was able to meet with visionary leadership who fully supported me. This hospital management assisted in every aspect from procuring equipment to recruiting motivated
team members, including trained nurses and interventional radiographers.
The clinical presence of IR is the need of the hour, especially when patients and other speciality doctors are looking for problem-solving skills and alternatives to surgical options. Now, patients can just walk in and consult an IR in the OP like any other speciality.
My suggestion to IRs starting a clinical practice is to strengthen your foundation by visiting different IR departments and learning about the workflow. Always try to learn a particular procedure from the best – at least a short observership during your practice is enough to boost your confidence.
Being an independent clinical department is the best thing you can do to your patients, to your speciality, and to yourself. It will ensure that IR is at its full potential and your patients will benefit tremendously.”