Symptoms
Prostate gland hypertrophy is related to lower urinary tract symptoms (also called LUTS), such as a urine stream that is hesitant, interrupted, or weak, and an urgent need to empty the bladder. Other symptoms include leaking, dribbling, feeling that the bladder is not empty after urinating and more frequent urination, especially at night.
Patients may also experience symptoms related to bacteria in the urine remaining in the bladder, such as frequent urinary tract infections and the development of bladder stones. In more severe cases, prostate gland hypertrophy may lead to urinary retention (being unable to urinate at all) and kidney failure, though this is less common.
Diagnosis
During the initial evaluation your doctor will ask you questions about your medical history and your urinary problems. The diagnostic work-up includes a digital rectal examination and testing your urine and blood.
You may have an ultrasound through your abdomen or rectum to calculate the size of your prostate and evaluate its structure. Ultrasound may also be used to calculate the residual urinary volume after urinating.
Treatment
Conservative treatment for prostate gland hypertrophy includes making changes to your lifestyle, such as reducing stress and avoiding drinking fluids in the evening. There are also several medications that may alleviate your urinary symptoms.
If conservative treatment does not work well, you may be advised to have a prostatectomy (the surgical removal of the prostate). This may be performed via open surgery or via transurethral resection. Transurethral resection is considered the treatment of choice and involves removing part of the prostate gland through the urethra. It is widely performed in patients not responding to conservative treatment. Complications of surgical treatments include urinary tract infections, narrowing in the affected area, post-operative pain, incontinence, sexual dysfunction and blood loss. There are also risks associated with the anaesthesia used during the procedure.
Alternatively, you may undergo a minimally invasive technique called prostate artery embolisation (PAE), which has been used to shrink the prostate gland with well demonstrated results. Prostatic artery embolization can be used also in cases where the prostate is too large for transurethral prostatectomy.
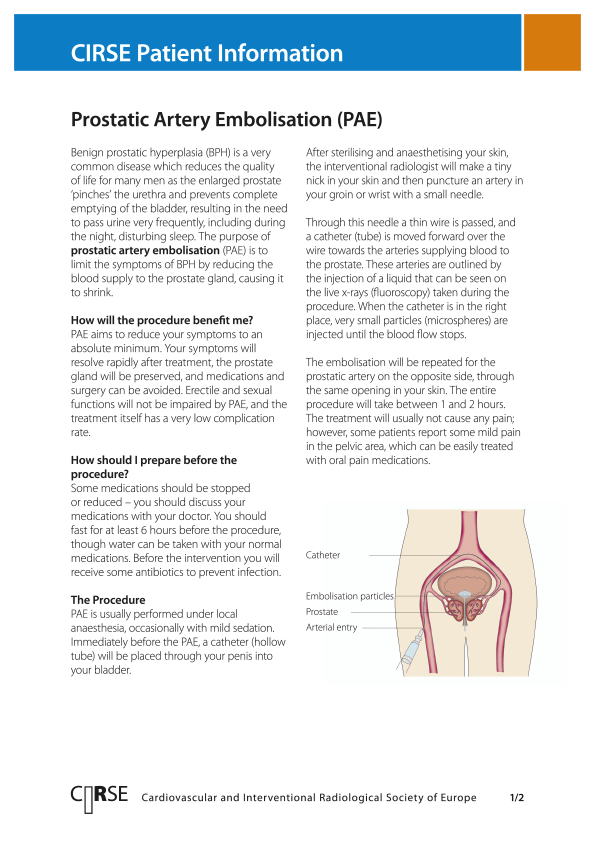
Prostatic artery embolization can be performed under local anaesthesia. During the procedure,after numbing the skin, an interventional radiologist inserts a small tube (catheter) through a blood vessel at the top of the thigh (or wrist). Under X-rays fluoroscopic guidance, they will direct the catheter to the prostatic artery and insert tiny biocompatible microspheres to block the artery that feeds the gland. This will cause the prostate gland to shrink. The procedure is usually performed on an out-patient basis and patients can resume normal activities immediately.
Bibliography
1. Pisco JM, Pinheiro LC, Bilhim T, et al. Prostatic Arterial Embolization to Treat Benign Prostatic Hyperplasia. Journal of Vascular and Interventional Radiology 2011; 22:11–19. PMID: 21195898.
2. Carnevale FC, Antunes AA, da Motta Leal Filho JM, et al. Prostatic Artery Embolization as a Primary Treatment for Benign Prostatic Hyperplasia: Preliminary Results in Two Patients. Cardiovascular Interventional Radiology 2010; 33:355–61. PMID: 19908092.