What is percutaneous image-guided jejunostomy?
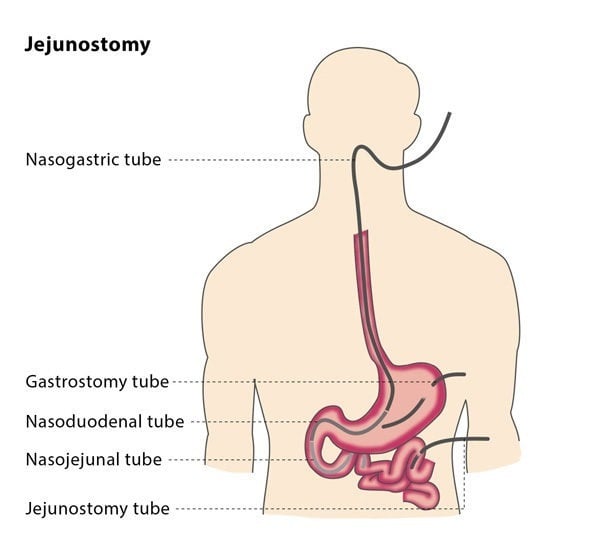
If you have been unable to eat for over seven days, you may need to receive nutrients intravenously (called parenteral feeding) or via a tube into the stomach or small bowel (called enteral feeding). There are a number of ways that enteral feeding can be carried out, such as placing a tube through the nose and into the stomach. This is called a nasogastric or nasoenteric feeding tube, and is the preferred option if your anticipated need is less than 30 days.
However, nasoenteric tubes are not suitable for use longer than 30 days, as they can cause considerable discomfort and complications such as inflamed sinuses. If your need is anticipated to be for longer than 30 days, a better option for you is direct enteral access. This involves placing a tube directly into your stomach or bowel. This used to require surgery, but minimally invasive techniques are now available as an alternative, such as percutaneous image-guided jejunostomy.
During a percutaneous image-guided jejunostomy, an interventional radiologist will place a tube directly through the abdominal wall and into part of your small intestine called the jejunum, providing a way for nutrients to enter your body.
How does the procedure work?
The procedure is carried out using fluoroscopic guidance. The interventional radiologist will first inflate your stomach using a nasogastric tube. This will aid the fluoroscopy, the required puncture and enlargement of the tract. In rare cases, nasogastric access may not be possible, so the stomach is inflated using a needle introduced into the stomach, under image guidance.