What is haemodialysis access maintenance?
Haemodialysis is a treatment in which a machine is used to filter out fluids and waste from the blood to restore a proper electrolyte balance in patients with kidney failure. There are three main access routes for this: intravenous catheters (thin plastic tubes which are placed in a blood vessel at the level of the shoulder or less often in the groin); arteriovenous (AV) fistulas, and synthetic grafts.
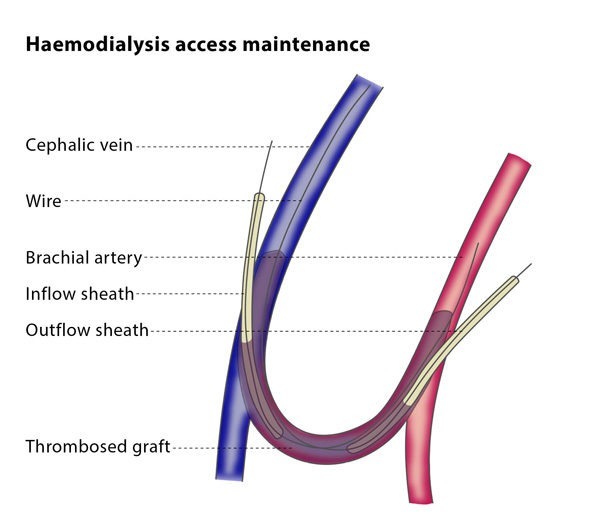
The most common vascular access method used is the AV fistula. This is a channel created by directly connecting an artery and a vein. A synthetic AV graft is small artificial tube placed under the skin connecting an artery to a vein, and tends to be used when the patient is unsuitable for an AV fistula.
Both AV fistulas and synthetic grafts may become narrowed, thrombosed (obstructed by blood clots) or blocked. In order to keep them clear, you may undergo a percutaneous (through your skin) treatment, such as percutaneous thrombolysis, thrombectomy, balloon angioplasty and stenting. The process of keeping the AV fistula or graft clear is called haemodialysis access maintenance.
How do the procedures work?
Haemodialysis access maintenance procedures are performed on an out-patient basis and use X-ray guidance. Your vital signs will be monitored during the procedure.